Let us first see what is Co-pay, Co insurance and Deductible
Co-payment
A co-payment, or co-pay, is the flat amount you pay at the time of a medical service or to receive a medication. All insurance companies provide these costs to you up front. Insurance companies use these co-pays in part to share expenses with you.
Co-pay example: A doctor’s office visit might have a co-pay of $30. The co-pay for an emergency room visit will usually cost more, such as $150. However, there is a maximum amount you will pay for coinsurance and co-pays. This is called the coinsurance and co-pay maximum.
Coinsurance
Coinsurance and co-payments are not the same thing. A co-payment is a specific amount that you pay to the provider before you meet your deductible. Coinsurance is a percentage of a provider’s charge that you may be required to pay after you’ve met the deductible.
Example of coinsurance: Say you’ve already paid out (or met) your $147 Medicare deductible and your coinsurance is 20 percent. For a $100 health care bill, you would pay $20 and your insurance company would pay $80.
When you’ve met your deductible, you’ll have to pay coinsurance (Medicare is set to 20 % of the provider’s charge) until you reach your out-of-pocket maximum. After that, the insurance company will pay for all covered services to the policy maximum for the remainder of the year
Deductible
A deductible is the amount you pay for health care services before your health insurance begins to pay. For Medicare, this resets every year on January 1st.
Part B Deductible for 2014: $147 per year (for most people).
Difference Between Co-pay and Coinsurance
Coinsurance: Coinsurance is a term used for a percentage amount you are responsible for. For example if your insurance policy is 80/20, then the insurance is 80%. You are responsible for paying 20% of your bill. The 20% that you owe is called "coinsurance." This amount can vary as the cost of the services performed varies.
Co-pay: A co-pay is usually a flat fee. For example, every time you go to the doctor you pay a 25.00 co-pay for the office visit, regardless of the level of service you receive.
While doing insurance Posting in PMS Software, line item may contain Co pay, Co Insurance and Deductible. The following are guidelines to handle the same.
PR - 1 Deductible Amount
Description:
In insurance policy terms, a deductible is the amount of money which the insured party must pay before the insurance company's own coverage plan begins. In practical terms, insurance companies include a deductible in their policies to avoid paying out benefits on relatively small claims.
Action:
1. We need to bill the patient.
2. If the patient has another insurance coverage which covers deductible we can file to that insurance, if the policy not cover primary deductibles we have no other way rather than billing the patient.
Claim processed as PR - 2 Coinsurance Amount
PR - 2 Coinsurance Amount
Coinsurance amounts are generally 20% of the Medicare fee schedule. Physicians must collect the unmet coinsurance from the beneficiary. Consistently waiving the coinsurance may be interpreted as program abuse. If a beneficiary is unable to pay the coinsurance, the physician should ask him or to sign a waiver that explains the financial hardship. If no waiver is signed, the beneficiary’s medical record should reflect normal and reasonable attempts to collect, before the charge is written off.
Action :
1. We need to file the claim to secondary insurance
2. If there is no secondary insurance we can bill the patient
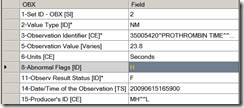
EOB - PR - 3 Co-payment Amount
PR - 3 Co-payment Amounts
Description:
Co-payment A specified dollar amount or percentage of the charge identified that is paid by a beneficiary at the time of service to a health care plan, physician, hospital, or other provider of care for covered service provided to the beneficiary.
Cost sharing the general set of financial arrangements whereby the consumer must pay out-of-pocket to receive care, either at the time of initiating care, or during the provision of health care services, or both. Cost sharing can also occur when an insured pays a portion of the monthly premium for heath care insurance.
Action:
1. We need to bill the patient.
2. If there is any other insurance coverage if the patient has, we can bill to that insurance also.
Co-pay Work Flow
Patient walks into doctor office .
People at the Reception desk ask the patient insurance card (it is like credit card) and see any amount mention in the card as co-pay. If not, they will do the eligibility check and see whether any co-pay is required. Insurance eligibility check will give the complete details where insurance is active , any co-pay amount to be paid, etc..
Once they determined, if co-pay amount need to be paid, then reception desk will do either of the following
Option 1: Will collect the amount and give the Patient receipt.
Option 2: Will Inform the patient that he/she need to pay copy after the Insurance payment is over. After insurance payment is over, we will send the patient statement to you and then you can pay your co- pay amount.
Option 3: Will inform the patient after the Insurance payment is over, we will send the claim to your secondary insurance and try to get the co-pay amount.
In most cases, doctor office will not collect the co-pay amount at the time of visit because either they may not known the exact amount or it may be cover by the secondary insurance. Please remember, the exact co-pay amount is calculated after insurance processing the claim and will be informed in the EOB.Billing company send the claim to Insurance company.
Insurance company process the claim and if any co-pay has to paid by patient, then they will mention that amount in the EOB.
Now the billing company transfer that amount from insurance side to patient side if patient does not have secondary insurance. (Move to Patient responsibility) if patient has secondary insurance, then they will send to secondary insurance and try to collect it from secondary insurance. Please remember, while sending the claim to secondary insurance, we must send the patient primary insurance information and what amount has been paid and what amount has been left over.
If secondary insurance does not cover that amount, then it will be transferred to patient responsibility.
Deductible Workflow
Simple example, once you taken the policy , insurance company says, first patient has to Pay $ 500 and then insurance will start paying for the medical services
1. Patient walks into doctor office A.
2. Doctor done some medical services to Patient.
3. Billing Department send the claim to Insurance. Let the bill amount is $ 200.
4. Insurance find that the patient has to pay $ 500 first and then they can start paying.
5. Now the insurance company send the EOB saying $200 is Deductible. Please note, here insurance company does not pay any amount. And also the insurance company system reduces this $ 200 from $ 500 and update the record balance as $300 deductible balance
6. Billing Department transfer this $ 200 to patient responsibility if the patient does not have secondary insurance. If the patient has secondary insurance, then claim send to secondary insurance for this amount.
**********************************
1. Same Patient walks into same doctor office A or doctor office B or lab.
2. Some medical Services done to Patient.
3. Billing Department send the claim to Insurance. Let the bill amount is $ 100
4. Insurance find that the patient has to pay $ 500 first and then they can start paying. And also records says $200 already met in the previous visit.
5. Now the insurance company send the EOB saying $100 is Deductible. Please note, here insurance company does not pay any amount.
And also the insurance company system reduces this $ 100 from $ 300 and update the record balance as $200 deductible balance.
6. Billing Department transfer this $ 100 to patient responsibility if the patient does not have secondary insurance. If the patient has secondary insurance, then claim send to secondary insurance for this amount.
**********************************
1. Same Patient walks into same doctor office A or doctor office B or lab.
2. Some medical Services done to Patient.
3. Billing Department send the claim to Insurance. Let the bill amount is $ 600
4. Insurance find that the patient has to pay $ 500 first and then they can start paying. And also records says $300 already met in the previous visit.
5. Now the insurance company send the EOB saying $200 is Deductible and Payment is $400
6. Billing Department transfer this $ 200 to patient responsibility if the patient does not have secondary insurance. If the patient has secondary insurance, then claim send to secondary insurance for this amount.
Questions or feedback are always welcome. You can email me at vbsenthilinnet@gmail.com