If you are new to Medical Billing, then please read this article first.
If you are new to EDI, then read the following articles
1. What is an EDI ?
2. EDI Transactions
3. Understanding EDI Structure
4. EDI Instruction
In the Medical Billing system, Process started from here and usually front desk people are doing this process. Its a process of verifying the patients insurance details by calling insurance or through online verification. If this department works well, we could resolve more problem. We have to do this even before patient appointment. Insurance verification can also be done using EDI transactions. Providers will initiate 270 transaction and insurance company responses with 271 transactions.
EDI 271 Transaction sent by insurance companies response to a 270 inquiry Transaction. This transaction is typically sent by insurance companies, government agencies like Medicare or Medicaid, or other organizations that would have information about a given policy. It is sent to healthcare service providers, such as hospitals or medical clinics that inquire to ascertain whether and to what extent a patient is covered for certain services.
What the response will contain ?
- Eligibility status
- Maximum benefits (policy limits)
- Exclusions
- In-plan/out-of-plan benefits
- C.O.B. information
- Deductible
- Co-pays
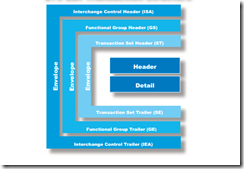
EDI 270 Structure
The 270 Eligibility, Coverage or Benefit t Inquiry Detail level contains all data relating to the requested transaction, including transaction participants, the subscriber, the dependent, and the patient detail information. Using a hierarchical level (HL) structure, the four levels for the participant types include:
Information Source Level : Loop 2000A
The Information Source is the payer that maintains the information regarding the patient’s coverage.NOTE! Information source does not refer to the entity sending the transaction.
Information Receiver Level : Loop 2000B
The Information Receiver is the entity requesting information regarding the patient’s coverage and is typically the medical service provider verifying insurance coverage for the patient.
Subscriber Level : Loop 2000C
The subscriber, who may or may not be the patient, is uniquely identified to an Information Source, traditionally referred to as a member.
Dependent Level : Loop 2000D
The dependent, who may or may not be the patient, is related to the subscriber.
EDI 270 Loops
1. Header Data – ISA, GS and BHT Loops
2. Information Source Level – Loop 2000A and Information Source Name – Loop 2100A
3. Information Receiver Level – Loop 2000B and Information Receiver Name – Loop 2100B
4. Subscriber Level – Loop 2000C and Subscriber Trace Number
5. Subscriber Name – Loop 2100C
6. Subscriber Demographic Information and Subscriber Date – Loop 2100C


No comments:
Post a Comment